
Uwe E. Reinhardt is an economics professor at Princeton. He has some financial interests in the health care field.
“In his writings, an Italian sage says that the best is the enemy of the good,” wrote Voltaire. We have updated that to the common adage, “Let not the perfect become the enemy of the good!”
Today’s Economist
Perspectives from expert contributors.
This dictum came to mind as I read the responses of various Doubting Thomases to my previous post on the quality of health care under the two Medicare options: traditional Medicare and Medicare Advantage.
These readers appear to harbor genuine doubt that quality in health care can ever be properly defined and measured. But what is the alternative — just relying on anecdotes and word of mouth, or the assurances from health care providers that they provide the highest quality of health care in the world?
It is, to be sure, challenging to measure the quality of any human-service sectors, be it health care, education, the administration of the law or even corporate management. That is why anecdotes and word of mouth remain important signals that attract or repel individuals from particular products or institutions.
But flight once seemed impossible, too, perhaps even after the Wright brothers’ first flight. “No flying machine will ever fly from New York to Paris,” Orville Wright famously said, because “no known motor can run at the requisite speed for four days without stopping.” Wright also offered the thought that “if we worked on the assumption that what is accepted as true really is true, then there would be little hope for advance.”
The large and growing cadre of clinicians and measurement scientists engaged in measuring quality in health care can find inspiration in aviation. They persist, and they have registered much more progress in recent decades than might be imagined — much more, for example, than has been achieved in other human-services sectors, notably education, not to mention what we call the administration of “justice.”
To appreciate the challenge posed by health care, let us review the huge terrain within which quality in health care can be monitored, an issue I touched upon two years ago in connection with “pay for performance.”
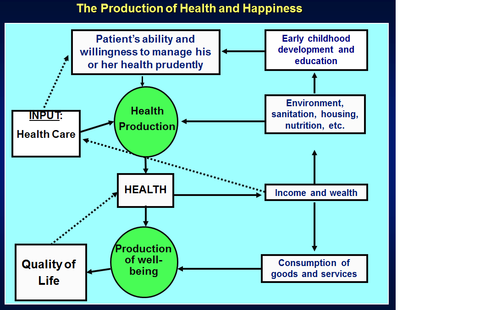
In that post, I presented a map of that terrain, reproduced here in modified form to highlight the three distinct though connected production processes in health care, as we economists put it:
(a) the production of health care (the gray area)
(b) the production of health (the blue area)
(c) the production of human well-being (the pink area)
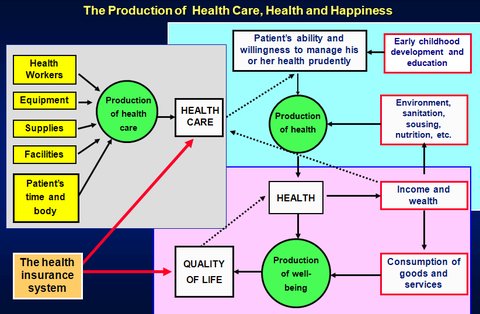
The ambition of measurement science devoted to quality in health care is to develop reliable and operational measures to monitor each of these production processes. It will be a quest that will last decades, and admittedly has only just begun.
The quality of health care production has naturally attracted most attention.
In the health care production process, quality can be monitored on several facets:
• The characteristics of the purchased inputs used in production of health care — e.g., the training of health personnel, the sophistication of the equipment supporting health professionals or the degree to which the architecture of facilities encourages or hinders patient-centered health care;
• The structure within which health care production takes place — e.g., the degree to which the production of health care is clinically integrated, including the electronic information technology that enhances or hinders that integration;
• The treatment processes for particular medical conditions — e.g., degree of adherence to known best clinical practices (expressed in practice guidelines and clinical pathways derived from these guidelines), processes that avoid hospital-generated infections and avoid re-admissions that could have been avoided, and so on;
• The impact of medical interventions on the patients’ health and well-being in the short and long run, often referred to simply as “outcomes” — e.g., survival rates by time periods, functional status, pain and so on;
• And, very important, satisfaction of patients with the treatment processes they have experienced, measured by means of surveys, ideally not administered by providers themselves.
This particular division of quality metrics goes back to a classic paper on the quality of health care published in 1966 by Dr. Avedis Donabedian, a distinguished physician and a towering figure in the field of quality measurement who died in 2000.
A wise thing to say in casual conversation is that “outcome” is all that matters in measuring the quality of health care. Presumably, “outcome” includes clinical outcome and patient satisfaction. Experts in quality measurement agree in principle. In practice, however, they warn that “outcome” is a complex metric.
First, clinical outcome usually is multidimensional. It may even involve a trade-off between longevity and quality of life.
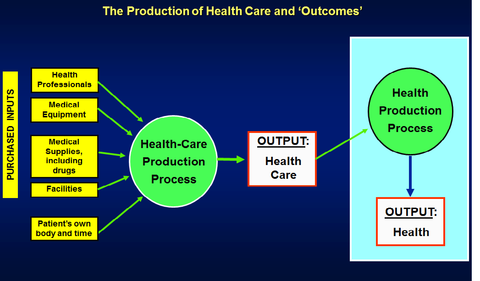
Second, as is shown in the next chart, which enlarges the health-production process, health care proper is merely an input in the production of health. To measure strictly the impact of a medical intervention on the patient’s health, one has to control statistically for all of these other health-producing inputs, including the patient’s compliance with, say, prescribed drug therapy, a perennial problem in health care.
Health care proper makes two inputs into the production of health: there may be intervention in the patient’s physiology – e.g., surgery, drug therapy, physical therapy or other direct interventions. But high-quality primary care also includes management-consulting services devised to help or persuade patients to manage their own health better — e.g., counseling on controlling blood pressure through methods besides drug therapy, nutrition, smoking cessation, weight management and so on. Modern metrics of quality monitoring always include a good number of metrics on these consulting services.
Efforts to hold health care providers formally accountable for the quality of their care are rarely one-metric systems. Instead, they resemble a final examination in a college course, with scores on many different questions, each with a relative weight, which are then totaled as a weighted sum to produce the final overall grade.
Quality monitoring I have seen from private insurers — e.g., Wellpoint Inc. or Massachusetts Blue Cross Blue Shield, to name but two — usually have scores on all of the several facets of quality enumerated above.
Ideally, it is these weighted sums that should be used in the kind of comparative analyses I mentioned in previous posts, rather than just hospital re-admissions. So far, these weighted aggregate measures have not been readily available to researchers — hence their reliance on single metrics on which data are available. One must hope that better data will soon be made available to researchers.
Article source: http://economix.blogs.nytimes.com/2013/02/01/measuring-the-quality-of-health-care/?partner=rss&emc=rss